
Advancing Digital Innovation to Reduce
Financial Toxicity in Cancer Care
Cancer is the 2nd leading cause of deaths in the U.S.
Among those that do survive, they are 2.5 times more likely to declare bankruptcy compared to those without a history of cancer.
Digital innovation holds promise to ensure access to quality care and reduce cost of cancer care.
Advancing Digital Innovation to Reduce Financial Toxicity in Cancer Care and Research
Digital innovation holds promise to ensure access to quality care and reduce cost of cancer care. This set of open-access resources helps health systems and their partners address barriers to implementing digital health tools in cancer care and research.
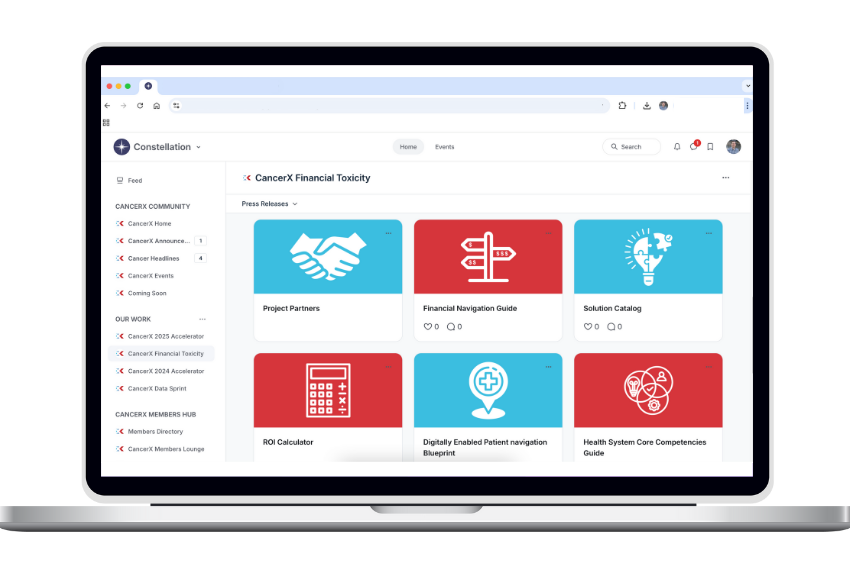
Use the solutions catalog, core competencies, and financial navigation guide, to implement digital solutions to improve healthcare access, cost, and clinical outcomes for your patients. And use the Digital Navigation ROI Calculator and Digitally Enabled Patient Navigation Blueprint to quantify and maximize the ROI of your investments in digitally enabled patient navigation.
By using these resources, you can unlock the promise of digital innovation to minimize challenges in cancer care access and out-of-pocket cost measures associated with cancer, ensuring that financial worries do not overshadow the fight for recovery.
Join our Community to engage with the Resources
You can create your profile for free to engage with our findings or view the solution catalog and use the ROI calculator. Already a member, simply login to view.
CREATE PROFILE
About Our Community
The CancerX Constellation is a online virtual community that provides oncology experts and healthcare leaders a private, exclusive environment to network, collaborate, engage in meaningful discussion and take part in CancerX Initiatives. You can create your own Follower profile for free to review and download all CancerX reports and findings.
Create Your Profile Now
Join the CancerX Constellation for free to view our Financial navigation Guide, Solutions Catalog, Patient Navigation Blueprint, Core Competency Guides and our ROI Calculator.
